A cutting-edge medical education
The Kaiser Permanente Mid-Atlantic States Internal Medicine Residency Program has an innovative and education-focused curriculum that puts strong emphasis on training to produce competent and resilient physicians. We use an innovative hybrid 4+2 and 2+2 block schedule, which provides a 50:50 inpatient and outpatient experience.
Listen to what Program Director Julie Chen has to say about how residents in the program will learn in our future-focused model of health care, and the benefits of being taught by our nationally recognized team of board-certified doctors.
Curriculum and rotations
Our innovative curriculum includes not only medicine, subspecialty topics, quality improvement, and research, but also chronic pain management, motivational interviewing techniques, nutrition and obesity medicine, excellence in physician-patient communication, and resident resilience and wellness.
| PGY-1 | PGY-2 | PGY-3 | |||
|---|---|---|---|---|---|
| Ambulatory block1 | 2 months | Ambulatory block1 | 2 months | Ambulatory block1 | 2 months |
| Core specialty rotations2 | 2 months | Core specialty rotations2 | 1 - 2 months | Core specialty rotations2 | 2 months |
| Inpatient medicine wards | 4 - 5 months | Inpatient medicine wards | 2 months | Inpatient medicine wards | 2 months |
| ICU | 1 month | ICU | 1.25 months | ICU | 1.5 months |
| Night medicine | 3 weeks | Night medicine | 1 month | CCU | 1 month |
| Neurology | 0.5 weeks | Non-medicine electives3 | 1 - 2 months | Night medicine | 0.5 month |
| Emergency medicine | 0.5 month | Advanced Urgent Care (AUC) | 0.5 month | Elective | 1 month |
| Vacation/Sick | 1 month | Vacation/Sick | 1 month | Neurology | 0.5 month |
| Emergency medicine | 0.5 month | ||||
| Vacation/Sick | 1 month | ||||
Disclaimer: This is a sample schedule
1Includes Underserved Medicine/social determinants of health rotation 2Core specialty rotations (Core specialty rotations 50:50 outpatient: inpatient balance): cardiology, endocrinology, gastroenterology, geriatrics, hematology-oncology, infectious diseases, nephrology, pulmonary disease, rheumatology 3Electives: advanced urgent care, allergy, away rotation, dermatology, gynecology, ENT, health information technology, health policy, lifestyle and culinary medicine, orthopedics, palliative care, POCUS, psychiatry, research, and sleep medicine.Quality improvement and patient safety
Quality improvement and patient safety will be an integral part of the bimonthly curriculum. Residents will have the opportunity to participate in the analysis of patient safety events. They will be required each year to design and participate in a quality improvement (QI) project. Residents will also be encouraged to present at the Morbidity and Mortality, Peer Review, Root Cause Analysis, and Sentinel Event Investigation conferences.
Wellness and resilience
The Residency Program has established a Resident Wellness Committee that emphasizes training and producing highly competent, resilient physicians by offering activities that focus on well-being. Planned activities include wellness weekends, resident and faculty retreats, reflective practice groups, didactics on wellness, and sessions on mindfulness, debt management, and more. The program’s structure ensures that residents’ work hours are well within limits for the ACGME requirements. Research shows that residents who work within restricted duty hours have much better wellness levels and less burn out. There is no overnight call in the resident schedule, though there are dedicated night float (inpatient wards) and night shifts (ICU) to ensure high-quality learning in the night medicine curriculum.
Sample didactics schedule
| Week 1 | Monday | Tuesday | Wednesday | Thursday | Friday |
|---|---|---|---|---|---|
| Ambulatory Conference 7:30 – 8 a.m. MKSAP Review 12 - 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 – 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 – 1 p.m. Academic Half-Day 1 – 5 p.m. | Ambulatory Conference 7:30 – 8 a.m. Board Review 12 - 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 - 1 p.m. | |
| Week 2 | Monday | Tuesday | Wednesday | Thursday | Friday |
|---|---|---|---|---|---|
| Ambulatory Conference 7:30 – 8 a.m. MKSAP Review 12 - 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 – 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 – 1 p.m. Academic Half-Day 1 – 5 p.m. | Ambulatory Conference 7:30 – 8 a.m. Board Review 12 - 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 - 1 p.m. | |
| Week 3 | Monday | Tuesday | Wednesday | Thursday | Friday |
|---|---|---|---|---|---|
| Ambulatory Conference 7:30 – 8 a.m. MKSAP Review 12 - 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 – 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 – 1 p.m. Academic Half-Day 1 – 5 p.m. | Ambulatory Conference 7:30 – 8 a.m. Board Review 12 - 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 - 1 p.m. | |
| Week 4 | Monday | Tuesday | Wednesday | Thursday | Friday |
|---|---|---|---|---|---|
| Ambulatory Conference 7:30 – 8 a.m. MKSAP Review 12 - 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Journal Club 12 – 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Grand Rounds 12 – 1 p.m. Academic Half-Day 1 – 5 p.m. | Ambulatory Conference 7:30 – 8 a.m. Board Review 12 – 1 p.m. | Ambulatory Conference 7:30 – 8 a.m. Noon Report 12 – 1 p.m. | |
Scheduled sessions
Noon Report
This conference is one of the most valuable educational sessions for our residents, and the residents are provided protected time from clinical duties. Our chief resident moderates case-based discussions, and interesting cases from both the inpatient and outpatient settings are presented. Residents and faculty engage in educational discussions at this daily teaching conference. M&M conferences, journal club, grand rounds, and conferences exploring high-value care and quality improvement will all be part of the bimonthly curriculum.
Academic Half-Day Conference
This weekly conference occurs every Wednesday and is a 4-hour block of protected time free from clinical duties. During this time, residents can focus on learning in a small group environment. Topics include general internal medicine, all subspecialties, evidence-based practice, humanism in medicine, and more.
Ambulatory Conference
Prior to every morning session of primary care clinic, residents participate in a protected half hour of didactic discussion on essential ambulatory topics with the faculty. The format varies to include case presentations, Yale modules, chart-stimulated recall, and chalk talks.
Ward attending team rounds
These small-group interactive teaching sessions will be based on patient cases from the inpatient teams. Team rounds will occur each morning after work rounds, or during the afternoon team meeting, and are facilitated by the attending hospitalist.
Intensive care rounds and teaching conference
Rounds are conducted each day with the ICU team by the intensivist at Holy Cross Hospital, along with short didactics in which essential topics in ICU medicine are covered systematically. Residents will undergo simulation training such as paracentesis and ultrasound-guided central line insertion.
Subspecialty rounds
Residents with subspecialty electives attend teaching and consultation rounds, which are conducted daily. Residents will work one-on-one with subspecialist faculty in the outpatient and inpatient settings during subspecialty rotations. They will also participate in subspecialty journal clubs, case review conferences, and tumor board, among other conferences.
What our residents have to say
The residency program has been supportive in helping me explore my interest in allergy and immunology. From flexible scheduling incorporating relevant electives to facilitating an invaluable away rotation, the program provided opportunities that were both formative and impactful. These experiences significantly deepened my understanding of the field and solidified my commitment to pursuing it. I am also sincerely grateful for the mentorship and guidance I received from faculty I met through these rotations, which have played a meaningful role in my growth.
Robert Liu, MD, PGY-3
Specialty training
Medicine wards
A wards team generally consists of an attending, one senior resident, and two interns. It may also include a sub-intern or a third-year medical student from an affiliated medical school like Penn State. Our call cycle consists of a recurring cycle with two days of “day-call” admitting, two “post-call” days with no admitting. There is no 24-hour call.
Specialty rotations
Each resident spends a two-week block in each of the core specialties of internal medicine both through our core subspecialty clinics and inpatient consultative services. These rotations are Monday through Friday in the outpatient setting, without weekend call or cross-coverage responsibilities.
Cardiology and CHF
Cardiology Clinic and Consultation will offer an exposure to diverse outpatient and inpatient populations with a variety of cardiac conditions. Residents on this rotation are exposed to interesting cardiology cases, including diagnoses of ischemic heart disease, heart failure, congestive heart failure and cardiomyopathies, valvular/structural heart disease, and common arrhythmias such as SVT, atrial fibrillation, ventricular tachyarrhythmias, and varying degrees of heart block. The rotation includes experience in the Advanced heart failure clinic and participation in cardiology testing and procedures (e.g., echocardiography, stress testing, ambulatory rhythm monitoring).
Pulmonology
The pulmonary rotation will provide residents with the necessary cognitive, technical, ethical, and social skills to manage several pulmonary conditions, including pulmonary medicine prevention, smoking cessation, vaccinations, screening and medication options for latent tuberculosis, evaluation of common pulmonary symptoms, obstructive airway disease, occupational and environmental lung disease, restrictive lung disease, interstitial lung disease, pulmonary hypertension, lower respiratory infections, pulmonary nodule, sleep medicine , positive pressure ventilation, pulmonary complications of HIV infection and opportunistic infections. This will also include pulmonary procedures such as the use of supplemental oxygen, spirometry, ABG, thoracentesis, and the administration of non-invasive positive pressure ventilation.
Nephrology
The nephrology rotation provides in-depth exposure and education for interested residents in areas of acid-base and electrolyte disorders, hypertension, and renal disease. Residents will care for and become adept at caring for outpatients with a variety of clinical conditions to include: hypertension, chronic kidney disease, and glomerular disease. On the inpatient consult service, residents will be exposed to a variety of consultative nephrology questions such as management of acute kidney injury, acid-base and fluid-electrolyte imbalance, and hemodialysis patients hospitalized for a variety of medical conditions.
Neurology
Residents will learn about neurology problems that are frequently seen in the primary care setting, as well as neurological diseases that are more frequently seen by neurology subspecialty services. They will become adept at evaluating a variety of neurological disorders, including but not limited to headaches, dizziness/vertigo, stroke, dementia and neurodegenerative disease (like motor neuron diseases), episodic conditions like epilepsy, demyelinating conditions, neuromuscular conditions, movement disorders like Parkinson’s disease, and neuro-oncological conditions. There will be opportunity to observe and participate in neurophysiology (EMG, EEG, Video EEG monitoring), botulinum toxin injections, nerve blocks, lumbar punctures, programming and interrogating vagal nerve stimulators, and deep brain stimulator procedures.
Endocrinology
Residents will be taught to diagnose and manage diabetes mellitus and other major hormonal imbalances and metabolism abnormalities; learn key clinical findings on physical examination of patients with common endocrine problems such as diabetes mellitus, hypogonadism, thyroid disorders, hypercalcemia, and hypoaldosteronism; and provide management for many interesting endocrine cases. They will also participate in procedures such as fine-needle biopsy of the thyroid, and ultrasound evaluation of the thyroid.
Rheumatology
Residents will learn about common and uncommon rheumatologic problems that are seen in the primary care setting. There will be opportunities to participate in injections of joints and bursa. The residents will be trained in the management of fibromyalgia, osteoarthritis, polymyalgia rheumatica, osteoporosis, gout, CPPD, myopathies, and a host of musculoskeletal disorders such as torn rotator cuff, knee internal derangement, cervical and lumbar spine radiculopathies, cauda equina, spondyloarthropathy, joint instability, inflammatory arthritides, and autoimmune conditions.
Gastroenterology
Residents work in the outpatient GI clinic and inpatient Gastroenterology & Hepatology disorders clinic with gastroenterologists. Here they learn the best practice guidelines, indications, risks, and benefits of tests and procedures that are frequently utilized in the diagnosis and management of patients with GI and liver disorders. Residents will assist with gastrointestinal procedures including upper and lower endoscopy, as well as advance endoscopy such as ERCP.
Hematology/Oncology
Residents will care for a diverse patient population with many types of hematologic and oncologic diseases. They will see a combination of new and follow-up patients to address a variety of hematology/oncology disorders and consultative issues. Residents will have the opportunity to observe and perform bone marrow biopsies, intrathecal delivery of chemotherapy, and accessing ports and PICC lines. Residents will also participate in tumor board discussions and work alongside the hematology/oncology physicians in the infusion center as part of the patient care team.
Away/audition rotations
The Internal Medicine Program and the department of Graduate Medical Education is supportive of away rotations, both at local institutions and institutions across the country.
Research rotations
Research blocks are available beginning PGY-2.
Resident as Teacher Curriculum
Residents have several opportunities to teach medical students who are rotating through Kaiser Permanente in both the inpatient and outpatient settings.
On the inpatient ward teaching team, the residents have the opportunity to work with sub-interns and third-year medical students from our affiliated institutions, including Penn State School of Medicine and Eastern Virginia Medical School. In the outpatient clinics, the residents work with and take part in teaching medical students from Georgetown and George Washington University.
At Kaiser Permanente of the Mid-Atlantic States, we’re proud to have highly qualified faculty who will mentor residents in research and quality improvement projects. Our physicians aspire to address the clinical, quality, and health policies that aim to improve the care experience of our patients and the communities we serve.
As a resident, you’ll have ample opportunities to collaborate with faculty on clinical trials and scholarly activities that will augment your training. Working on these projects will better prepare all of our residents to pursue scholarship and research activities for the advancement of medical care.

Training locations

Gaithersburg Medical Center
655 Watkins Mills Road
Gaithersburg, MD 20877
Gaithersburg Medical Center will serve as the primary outpatient clinical site for the longitudinal continuity experience, ambulatory medical subspecialties, and non-medicine electives (ophthalmology, physical therapy, gynecology, etc.) for the Kaiser Permanente Mid-Atlantic States Internal Medicine Residency Program. The facility is equipped with a laboratory, full range of radiology services, and pharmacy, along with an Advanced Urgent Care (AUC) capable of overnight observation for cardiac monitoring and advanced imaging. The center sees over 400 diverse patients daily, with a wide range of pathology. In addition to medical specialties, Gaithersburg Medical Center houses surgical and other specialties.
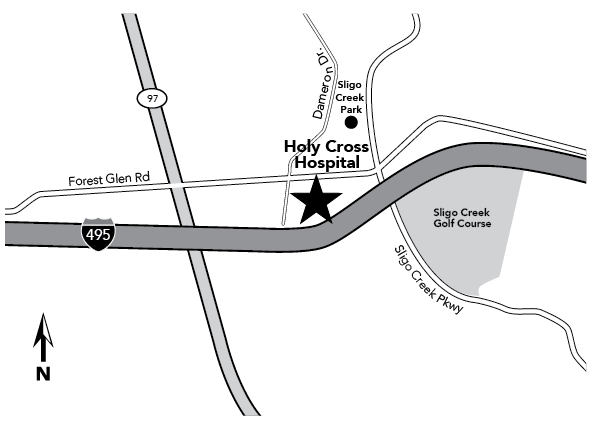
Holy Cross Hospital
1500 Forest Glen Road
Silver Spring, MD 20910
Holy Cross Hospital in Silver Spring, Maryland, is a 455-bed, not-for-profit teaching hospital that serves as our main inpatient resident training site. Holy Cross is staffed by devoted hospitalists, intensivists, and emergency medicine physicians who are dedicated clinician educators for the residency program. The hospital will provide clinical experiences in inpatient medicine, emergency medicine, subspecialty medicine, and critical care experiences with 24/7 hospitalists and emergency medicine physicians serving as in-house faculty supervisors.
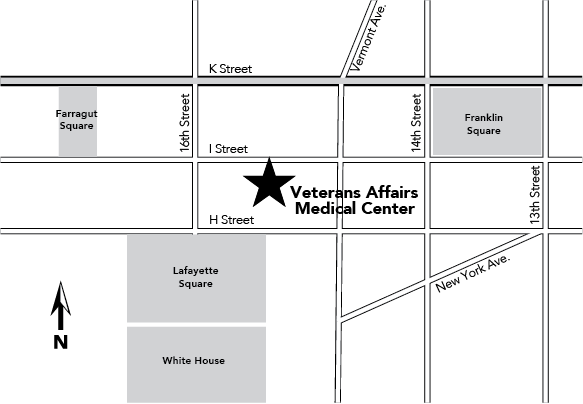
Veterans Affairs Medical Center
50 Irving Street NW
Washington, DC 20422
The Veterans Affairs Medical Center has an in-depth program in geriatrics. Residents will have clinical rotations in the geriatrics clinic, geriatrics and palliative medicine consult service, nursing home care unit, inpatient rehabilitation services, and geropsychiatry. Seven geriatricians serve as primary faculty in collaboration with multiple interdisciplinary teams to provide a broad variety of clinical and academic training.
Explore Gaithersburg Medical Center
Explore Holy Cross Hospital
Salary & benefits
Aside from the competitive salary, the Kaiser Permanente Mid-Atlantic States Internal Medicine Residency Program offers residents health and dental insurance, professional liability coverage, life and disability insurance, a tax-sheltered annuity option, an educational stipend, paid time off, and a wide variety of discounts including fitness, childcare services, parent medical coverage, and more.
Each resident will also receive an educational fund which can be used for medical supplies or conference attendance. In addition, a free subscription to UpToDate®, AMBOSS, access to a full clinical library of textbooks and journals, and membership in the American College of Physicians, including MKSAP, is provided for each resident.
For a comprehensive look at program benefits, click here.
For terms and conditions of the residency program, click here.
| PGY-Level | 2025 Salary |
|---|---|
| PGY-1 | $71,526.05 |
| PGY-2 | $73,442.91 |
| PGY-3 | $77,755.41 |
Other benefits include:
- Smartphone and laptop pre-loaded with state-of-the-art applications used for daily clinical activities in the program
- Paid licensure fees
- Transportation vouchers for long call shifts
- Lunch allowance Monday to Friday during noon conference
Are you a good fit for our program?
The Kaiser Permanente Mid-Atlantic States Internal Medicine Residency Program is seeking candidates who share Kaiser Permanente’s commitment and passion for bringing high-quality, patient-centered care to the community in an accessible, cost-effective manner. Part of the foundation of our program is preparing you to work to improve and advocate for quality patient care and patient safety. If you agree that health care must be affordable for all — because thriving individuals, families, and communities require that — you’ll be at home in the Kaiser Permanente Mid-Atlantic States Internal Medicine Residency Program.
As a resident in our program, you’ll remember the reason you chose medicine as a profession. You’ll learn to practice medicine in a program that’s committed to providing high-quality health care through ongoing research and innovation, so you’re better prepared to deliver more efficient and meaningful care experiences. In joining the Kaiser Permanente Mid-Atlantic States Internal Residency Program, you’ll be part of a movement that understands that being healthy is about taking care of the whole you — mind, body, and spirit.
You’ll also get to support Kaiser Permanente’s mission to improve the health of the communities we serve by volunteering at local health fairs and special events across the region. Our efforts focus on implementing population-based health initiatives that will help make Kaiser Permanente communities among the healthiest in the nation. You’ll be part of an organization that works to improve community health through the use of programs, grants, social impact investments, and policy advocacy that increase access to quality care, create economic and educational opportunities, and enhance community environments.
Residents in our program will demonstrate certain core professional and personal characteristics and values, including:
- Integrity
- Commitment to excellence
- Efficient use of time and resources
- A shared sense of responsibility
- Flexibility
- Respectfulness
- Ability to embrace and accept cultural diversity
- Reliability
- Innovative problem-solving skills
- Responsiveness to constructive criticism
- Compassion
- The highest professionalism
- Quality with consistent standards
If you believe you have these attributes and want to launch a fulfilling medical career in an environment that supports you, we encourage you to apply to the Kaiser Permanente Mid-Atlantic States Internal Medicine Residency Program.
